Acas Carotid Trial
PubMed • Full text
Purpose: Proponents of carotid angioplasty and stenting suggest that “high risk” patients, defined as patients excluded from the North American Symptomatic Carotid Endarterectomy Trial (NASCET) and Asymptomatic Carotid Atherosclerosis Study (ACAS), may have a significantly higher risk of stroke with carotid endarterectomy (CEA). THE NASCET 1 and the ACAS 2 were the largest and best-organized trials affecting the management of extracranial carotid arteriosclerosis. Both trials have clearly defined patient populations that benefit from carotid endarterectomy compared with best medical management.
- 6Population
- 8Outcomes
Clinical Question
Does carotid endarterectomy (CEA) and aggressive medical therapy reduce incidence of cerebral infarction over 5 years in patients with asymptomatic carotid artery stenosis?
Bottom Line
Patients with asymptomatic carotid artery stenosis of 60% or greater who are good surgical candidates have reduced 5-year risk of ipsilateral stroke.
Major Points
While the NASCET trial showed the benefit of CEA for patients symptomatic from carotid artery stenosis, the Asymptomatic Carotid Atherosclerosis Study (ACAS) trial sought to test whether a morbidity and mortality benefit existed for treated asymptomatic patients with CEA. ACAS demonstrated that asymptomatic patients with carotid artery stenosis >60% who undergo CEA have a lower chance of a combined endpoint of ipsilateral stroke, or perioperative stroke or death over 5 years.
Guidelines
No guidelines have been published that reflect the results of this trial.
Design
- 39 center trial
- Non-blinded
- Randomized
- N=1,662
- Aggressive Medical Therapy alone (n=834)
- Aggressive Medical Therapy + Carotid Endarterectomy (n=825)
- Enrollment: December 1987 to December 1993.
- Median follow-up: 2.7 years
- Analysis: Intention-to-treat
Population
Inclusion Criteria
- Aged 40-79
- Compatible history and findings on physical and neurological exams
- Performance of required lab and ECG testings no earlier than 3 months prior to randomization
- Patient accessibility and willingness to be followed for 5 years
- Valid informed consent
Acas Carotid Trial Meaning

Exclusion Criteria
- Cerebrovascular events in the distribution of the study carotid artery
- Cerebrovascular events in the distribution of the vertebrobasilar arterial system
- Symptoms referable to the contralateral hemisphere within the previous 45 days
- Contraindications to aspirin
- Disorder that seriously complicate surgery
- Condition that would prevent continuing participation, or that would likely produce disability or death within 5 years)
Baseline Characteristics
- Gender: Approximately 2 Male:1 Female
- Age
- 40-49: ~2%
- 50-59: ~14%
- 60-69: ~48%
- 70-79: ~37%
- Percent Stenosis
- 0-59%: NA
- 60-69%: ~36%
- 70-79%: ~37%
- 80-80%: ~25%
- 90-99%: ~5%
Acas Carotid Trial
Interventions
- 'Aggressive Medical Therapy': 325mg of regular or enteric-coated aspiring daily and 'modification of stroke risk factors'
- 'Aggressive Medical Therapy' Plus Carotid Endarterectomy
Outcomes
Comparisons are Medical versus Surgery
Primary Outcomes
- Ipsilateral Stroke or any perioperative stroke or death
- 11.0% v 5.1% (p=0.004)
Secondary Outcomes
- Major Ipsilateral Stroke or any perioperative major stroke or death
- 6.0% v 3.4% (p=0.12)
- Ipsilateral TIA or Stroke or any perioperative TIA or stroke or death
- 19.2% v 8.2% (p<0.001)
- Any stroke or any perioperative death)
- 17.5% v 12.4% (p=0.09)
- Any major stroke or perioperative death
- 9.1% v 6.4% (p=0.26)
- Any stroke or death
- 31.9% v 25.6% (p=0.08)

- Any major stroke or death
- 25.5% v 20.7% (p=0.16)
Subgroup Analysis
Reduction due to Surgery in 5 year risk as a proportion of risk in the medical group
- By Sex
- Men: 0.66 (95% CI: 0.36 to 0.82)
- Women: 0.17 (95% CI: -0.96 to 0.65)
- By Age
- < 68 y.o.: 0.60 (95% CI: 0.11 to 0.82)
- >= 68 y.o.: 0.43 (95% CI: -0.07 to 0.70)
Acas Carotid Trial Procedure
- By history
- Bilaterally asymptomatic: 0.46 (95% CI: 0.00 to 0.71)
- Previous Contralateral endarterectomy or previous TIA or stroke: 0.65 (95% CI: 0.13 to 0.86)
- Protocol adherence
- Patients receiving assigned treatment: 0.55 (95% CI: 0.23 to 0.74)
- By degree of Stenosis
- 60-69.9%: 0.45 (95% CI: -0.70 to 0.82)
- 70-79.9%: 0.67 (95% CI: -0.65 to 0.94)
- 80-99.9%: 0.45 (95% CI: -2.19 to 0.91)
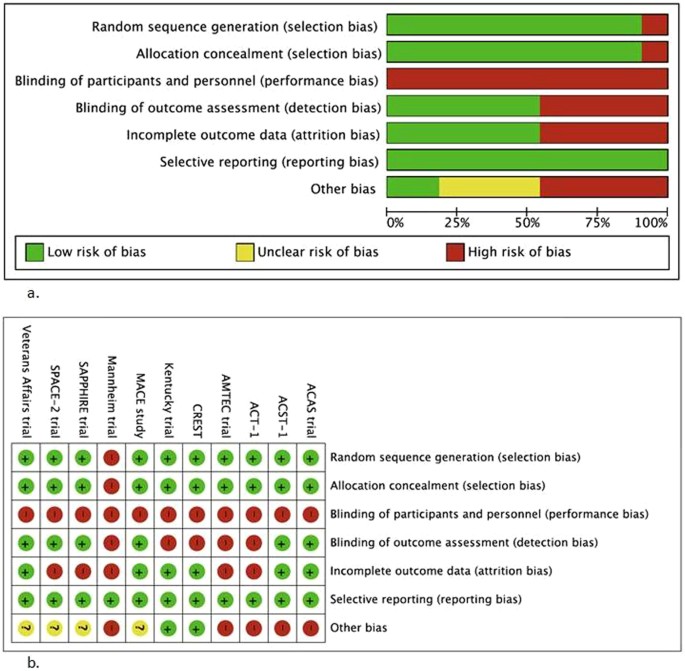
Criticisms
- This study relied heavily on composite endpoints for all endpoints, which may not be statistically rigorous.
- 'Aggressive Medical Therapy' in 1995 consisted on aspirin alone, whereas modern clinical guidelines demand treating patients with atherosclerotic disease with a statin. Additionally, modern medical therapy includes management of comorbidities such as hypertension and diabetes mellitus, but newer medications have improved efficacy, which may affect how effective medical management can be.
Funding
- This study was funded by the National Institutes of Neurological Disorders and Stroke, NIH.
- A conflict of interest may exist because the study was examining the clinical effectiveness of a surgical intervention by vascular surgeons, when these very physicians are those whose careers will suffer if CEA proved to be inferior.