5 Roots In Molar
| Maxillary first molar | |
|---|---|
Maxillary first molars of permanent and primary teeth marked in red. | |
| Identifiers | |
| FMA | 290269 |
| Anatomical terminology | |
- 5 Roots In Tooth
- 5 Roots In Molar Mass
- 5 Roots In Molar Extraction
- 5 Roots In Molar Formula
- 5 Roots In Molars
- 5 Roots In A Molar
Video description[edit]
Introduction[edit]
5 Roots In Tooth
The maxillary first molar is the human tooth located laterally (away from the midline of the face) from both the maxillary second premolars of the mouth but mesial (toward the midline of the face) from both maxillary second molars.
The function of this molar is similar to that of all molars in regard to grinding being the principal action during mastication, commonly known as chewing.
There are usually four cusps on maxillary molars, two on the buccal (side nearest the cheek) and two palatal (side nearest the palate). There may also be a fifth smaller cusp on the palatal side known as the Cusp of Carabelli.
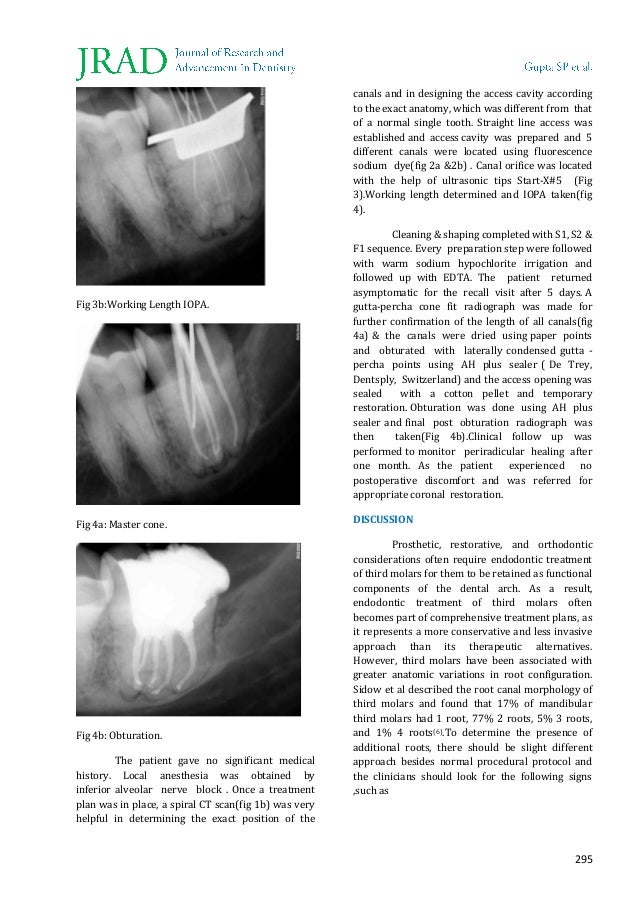
Four percent of teeth have only two roots. The broad bucco-lingual dimension of the mesio-buccal root and associated concavities on the mesial and distal surface is consistent with the majority of mesio-buccal roots having two canals. The incidence of root fusion of two or three roots is approximately 5.2%. The crown of the molars has modified into an occlusal (chewing) surface with 3 to 5 cusps. Moreover, the occlusal surfaces of molars are larger than that of other teeth. The main roles of molars include the mastication of food, maintenance of vertical dimension of the face, and help to keep other teeth in proper alignment. Dentin composes most of the root, which normally has pulp canals. The roots of teeth may be single in number (single-rooted teeth) or multiple. Canines and most premolars, except for maxillary first premolars, usually have one root. Maxillary first premolars and mandibular molars usually have two roots. Maxillary molars usually have three roots. A root fracture of a permanent tooth is commonly referred to as a vertical root fracture and it usually consists of a crack that appears on the root of the tooth below the gum line. Occasionally, the fracture will spread up the natural tooth appearing above the gum line where there is then the risk of a complete split.
Normally, maxillary molars have four lobes, two buccal and two lingual, which are named in the same manner as the cusps that represent them (mesiobuccal, distobuccal, mesiolingual, and distolingual lobes). Unlike the anterior teeth and premolars, molars do not exhibit facial developmental depressions. Evidence of lobe separation can be found in the central groove, which divides buccal from lingual lobes. The two lingual lobes are separated by the distolingual groove, and the two buccal lobes are divided by the buccal groove.[1]
There are great differences between the deciduous (baby) maxillary molars and those of the permanent maxillary molars, even though their function are similar. The permanent maxillary molars are not considered to have any teeth that precede it. Despite being named molars, the deciduous molars are followed by permanent premolars.
Notation[edit]
Permanent maxillary first molar notation
In the universal numbering system, one number is used to identify the tooth. The right permanent maxillary first molar is known as tooth '3', and the left permanent maxillary first molar is known as tooth '14'.
In the Palmer notation, a number and symbol are used to identify the tooth. The number identifies the tooth position relative to the midline, and the symbol identifies the quadrant of the mouth. Both maxillary first molars have the same number; 6. However, the right molar has the symbol '┘' underneath it. The left molar has '└' underneath it.
In the international system of notation two numbers are used to identify the tooth. The first number identifies the quadrant of the mouth. The second number identifies the tooth relative to the midline of the arch. The right permanent maxillary first molar is known as '16'. The left permanent maxillary first molar is known as '26'.
Deciduous maxillary first molar notation
In the universal numbering system, an uppercase letter is used to identify the tooth. The right deciduous maxillary first molar is known as 'B', and the left one is known as 'I'.
In the Palmer notation, a letter and symbol are used to identify the tooth. The letter identifies the tooth position relative to the midline, and the symbol identifies the quadrant of the mouth. Both maxillary first molars have the same letter; 'D'. However, the right molar has the symbol '┘' underneath it. The left molar has '└' underneath it.
In the international system of notation two numbers are used to identify the tooth. The right deciduous maxillary first molar is known as '54', and the left one is known as '64'.
External root morphology[edit]
The maxillary first molar normally has three roots.
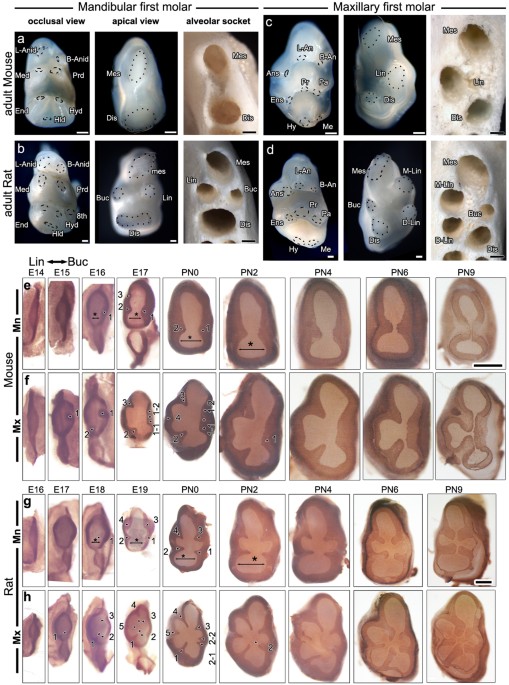
- The mesiobuccal root is broad distobuccal and has prominent depressions or flutings on its mesial and distal surfaces. The internal canal morphology is highly variable, but the majority of the mesiobuccal roots contain two canals.
- The distobuccal root is generally rounded or ovoid in cross section and usually contains a single canal.
- The palatal root is more broad mesiodistally than buccolingually and ovoidal in shape but normally contains only a single canal. Although the palatal root generally appears straight on radiographs, there is usually a buccal curvature in the apical third. Depressions on the buccal and palatal surfaces of the palatal root can be present but are generally shallow.
There are prominent depressions found on the distal aspect of the mesiobuccal roots. Depressions can also be found on the furcal side of the distobuccal and palatal roots.
The overall average length of the maxillary first molar is 20.5 mm with an average crown length of 7.5 mm and an average root length of 13 mm.[2]
Pathologies[edit]
The maxillary first molars are the second most common carious teeth and the second most common teeth to undergo endodontic treatment or extraction (with mandibular first molars the most common diseased teeth). Up to 21% of all extracted teeth are maxillary first molars.[3]
References[edit]
- ^Ash, Major M.; Nelson, Stanley J. (2003). Wheeler’s Dental Anatomy, Physiology, and Occlusion (8th ed.). ISBN0-7216-9382-2.
- ^J. Craig Baumgartner MS, DDS, PHD, John I. Ingle, DDS, MSD, Leif K. Bakland, DDS, eds. 2008. Ingle's Endodontics. Hamilton, Ontario. BC Decker Inc. ISBN0-19-920409-8, ISBN1-55009-333-9.
- ^Zadik Y, Sandler V, Bechor R, Salehrabi R (August 2008). 'Analysis of factors related to extraction of endodontically treated teeth'. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 106 (5): e31. doi:10.1016/j.tripleo.2008.06.017. PMID18718782.
One of the most dreaded medical procedures is having a tooth extracted. The thought of sitting in a dentist's chair under anesthesia scares some people more than the bloodiest horror film. But it's not nearly as horrific as it sounds. Tooth and tooth root extraction is a common surgery, one with few complications and minimal pain.
A tooth may have to be extracted due to various dental concerns. Periodontal disease, also known as advanced gingivitis, can cause a tooth to become separated from the gum and bone that holds the tooth within the socket [source: WebMD]. Once this happens, the tooth needs to be removed to prevent even more infection. Also, if you play a sport or sustain an injury to the mouth, one or more teeth can be knocked loose to the point that they need to be taken out avoid further complications.
Advertisement
Advertisement
There are also basic orthodontic reasons to have a tooth extracted. Baby teeth that crowd a mouth often mean adult teeth will also be crowded. And while some people seem to have enough room in their mouths for wisdom teeth to come through completely, dentists often extract them because they're difficult to reach with a toothbrush and floss, which increases the risk of tooth decay.
Other reasons why a person may have a tooth extracted include [source: Colgate]:
- A person who has a high risk of infection due to an organ transplant, receiving cancer drugs or is under immunosuppressive therapy. People with transplants or serious illnesses are highly susceptible to infection. Even if there's only a small chance a tooth may become a problem, it must be taken care of immediately.
- Children needing braces may need baby teeth removed to help their adult teeth come in straight. This is sometimes considered a cosmetic procedure, but it allows for braces to work more efficiently.
Both baby and adult teeth 'erupt' (the formal name for teeth coming in the mouth) when they come all the way in through the gums. According to Dr. Jeremy Rosenberg, a dentist in Atlanta, Ga., teeth that need to be extracted fall into two categories -- fully impacted or partially impacted. Full impaction means the tooth is under the gum and completely covered by the jawbone. A partially impacted tooth means the tooth is partially covered by some bone and gum tissue. A tooth is always completely removed, roots and all. Dr. Rosenberg said that occasionally, a small fragment of root may break off and is left in the bone if it will cause trauma to the area to remove it. He explained that the body forms bone around it and heals normally. However, this doesn't happen often, and the root piece has to be very small to be left in the mouth.

Now you know why teeth are extracted. On the next page, learn how they're removed and by whom.
Advertisement
A general dentist or specialized surgeon of the mouth, called an oral or maxillofacial surgeon, will perform tooth and tooth root extractions [source: WebMD]. Some general dentists don't like to extract teeth, so they'll refer all extractions to an oral surgeon. Periodontists (dentists who specialize in treating periodontal disease) and cosmetic dentists may also perform tooth extractions [source: AAP].
Your dentist or oral surgeon will first determine the difficulty of the tooth extraction, based on the condition and position of the tooth (such as if it's fully or partially impacted). A tooth with advanced periodontal disease, for example, is easier to extract than a healthy tooth with long roots because the tooth and gums surrounding it have deteriorated so much. Wisdom teeth generally have their own issues for removal, including teeth that have already come through the gums; soft-tissue impaction, where the tooth is lying under the gum; partial-bony impacted, where the tooth is partially erupted and partially stuck in the jaw; and full-bony impacted, where the tooth is completely stuck in the jaw [source: WebMD].
Advertisement
Advertisement
There are two types of tooth and tooth root removal procedures. The first one is called a simple extraction, which is performed on a tooth that has already erupted. A dentist uses forceps or a 'dental elevator' placed between the gum and tooth, to loosen it and remove it completely [source: Colgate]. There is usually no cutting into the gum during this procedure. The second type of tooth removal is called a 'surgical extraction,' where an oral surgeon needs to cut into the gum line to expose the tooth and roots for extraction.
Most tooth extractions are done with the same local anesthetic used when filling a cavity. According to Dr. Rosenberg, it's usually up to the patient to decide if he prefers sedation in addition to local anesthesia. Sedation methods include nitrous oxide (commonly known as laughing gas), an IV sedative that goes directly into the patient's bloodstream or an oral sedative [source: WebMD]. A dentist may recommend general anesthesia instead of local if several teeth will be removed in the same surgery or if the patient has significant anxiety over the procedure. If general anesthesia is used, another person is needed to accompany the patient home after the procedure.
5 Roots In Molar Mass
Next up, learn how to care for your mouth after a tooth has been removed.
Advertisement
Overall, there isn't much risk associated with tooth extractions, but as with any medical procedure, there is always the chance of complications. With tooth extraction, complications may include delayed healing, infection, numbness of the mouth and dry sockets. With a dry socket, the protective blood clot that forms over the extraction site either dissolves or moves, which leaves the tooth socket (or bone) exposed to everything you put in your mouth, and can be extremely painful [source: WebMD]. Dry sockets are treated with pain relievers, rinses or other treatments from your dentist.
There is a standard after-care regimen for patients who have teeth extracted. Dr. Rosenberg recommends that patients gently bite down on gauze to stop any bleeding post-surgery and then begin saltwater rinses the day after extraction. He also advises patients to continuing rinsing after each meal for a week or two after surgery, which will kill bacteria and flush any food debris that may get stuck in the extraction site. Antibiotics and pain medicine may also be given if the person needs it; otherwise, it's just a matter of time for the body to heal itself.
Advertisement
Advertisement
Other things you can to do make sure your mouth heals properly include [source: ADA]:
- Eat soft foods and liquids such as soup, gelatin, oatmeal and pudding for a couple of days. This will allow the site to heal without traumatizing the extraction site through biting or chewing.
- Avoid smoking and using straws (sucking in air can be painful to the wound and lead to dry sockets).
- Gently brush your teeth, and avoid directly brushing the healing socket until you feel the area is strong enough for full pressure.
5 Roots In Molar Extraction
Advertisement
5 Roots In Molar Formula
Related Articles
5 Roots In Molars
Sources
5 Roots In A Molar
- American Academy of Periodontology (AAP). 'What is a Periodontist?' (Sept. 29, 2011) http://www.perio.org/consumer/periodontist2.htm
- American Dental Association (ADA). 'Tooth Extraction.' (Sept. 8, 2011) http://www.ada.org/2926.aspx
- Colgate. 'Tooth Extraction.' (Sept. 20, 2011) http://www.colgate.com/app/CP/US/EN/OC/Information/Articles/Oral-and-Dental-Health-Basics/Checkups-and-Dental-Procedures/Tooth-Removal-Extraction/article/Tooth-Extraction.cvsp
- Edmonds, Molly. 'Are people without wisdom teeth more highly evolved?' (Sept. 29, 2011) https://health.howstuffworks.com/human-body/parts/no-wisdom-teeth2.htm
- Rosenberg, Jeremy, D.D.S. Dentist in Atlanta, Ga. Personal correspondence. Sept. 18, 2011.
- WebMD. 'An Overview of Dry Socket.' (Sept. 29, 2011) http://www.webmd.com/oral-health/dry-socket-symptoms-and-treatment
- WebMD. 'Dental Health and Wisdom Teeth.' (Sept. 29, 2011) http://www.webmd.com/oral-health/guide/wisdom-teeth
- WebMD. 'Gingivitis and Periodontal Disease (Gum Disease)' (Sept. 29, 2011) http://www.webmd.com/oral-health/guide/gingivitis-periodontal-disease
- WebMD. 'Tooth Extraction.' (Sept. 29, 2011) http://www.webmd.com/oral-health/tooth-extraction